A report by the Wellcome Trust — for which 10,000 people in 12 countries were queried — has revealed that most people are "alarmingly confused" about the use and consequences of taking antibiotics:
- 64 percent of people wrongly believe that antibiotics treat viral infections such as colds and flu
- 75 percent of people wrongly believe "antibiotic resistance" means that your body is resistant to the drug rather than the bacteria being resistant
- About one-third of people wrongly believe you should stop taking the antibiotic once you feel better to avoid building "immunity" to the drug
- 66 percent wrongly believe you're not at risk of drug-resistant infection as long as you follow your doctor’s prescription
- Nearly half wrongly believe drug-resistant infections affect people who use antibiotics frequently when in fact they can affect anyone
The facts are:
- Antibiotics can ONLY treat bacterial infections. They have no effect on viral infections including colds and flu
- Unless the disease-causing bacteria are completely wiped out, the infection may recur, so it's important to finish the entire course
- Antibiotics should be reserved for SEVERE bacterial infections and only as a last resort
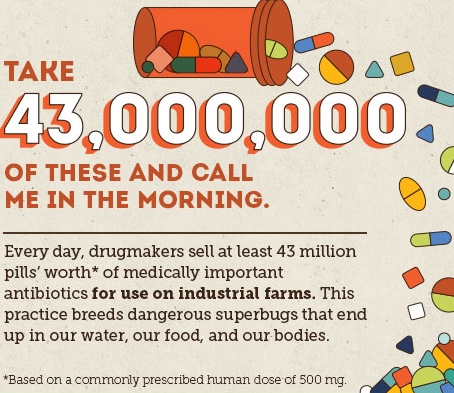
- Non organic meat and dairy from intensely raised animals and fish are major sources of antibiotics that will make their way to our body. Antibiotics are used as prophylactics (and convenient growth promoters) because stressed animals forced to live in confined spaces are prone to disease. Only choose organic, wild or traceable meat, dairy and fish to avoid unnecessary exposure to antibiotic.
This makes a convincing argument for educating ourselves better about antibiotics, their use and associated risks, if we are to continue enjoying the current level of protection they offer
Gut flora is especially vulnerable to antibiotics
Research in the UK and Sweden has revealed that, depending on the type, antibiotic treatments can affect gut microbiome adversely for up to a year afterwards.
The randomized, placebo-controlled clinical trial evaluated participants' oral and gut microbiomes.
The oral microbiome normalized fairly quickly, but the gut microbiome typically did not.
As reported by The Atlantic:
"People who took clindamycin and ciprofloxacin saw a decrease in types of bacteria that produce butyrate, a fatty acid that lowers oxidative stress and inflammation in the intestines. The reduced microbiome diversity for clindamycin-takers lasted up to four months; for some who took ciprofloxacin, it was still going on at the 12-month check-up. Amoxicillin, on the plus side, seemed to have no significant effect on either the oral or gut microbiome, and minocycline-takers were back to normal at the one-month check-up."
The study also demonstrated that the risk of antibiotic-resistant disease is increased:
- Antibiotic-resistance genes were found in both British and Swedish participants at the outset of the study, although the British had on average a 1.13-times-higher load of antibiotic resistance genes than the Swedes. (The authors speculate that this may be a result of the fact that Sweden has significantly decreased use of antibiotics over the past 20 years, due to the Swedish Strategic Program for the Rational Use of Antimicrobial Agents and Surveillance of Resistance [STRAMA], launched in 1994.)
After exposure to antibiotics, the antibiotic resistance gene load increased across the board.
According to the authors:
"Among the antibiotics tested, exposure to amoxicillin resulted in the least discernible effects on the microbiome composition, while these samples had the highest number with antibiotic resistance-associated genes and the most classes that were increased in the predicted metagenomes and in the full metagenomes, respectively, a week after the exposure ...
Clearly, even a single antibiotic treatment in healthy individuals contributes to the risk of resistance development and leads to long-lasting detrimental shifts in the gut microbiome."
Antibiotics save lives. I am not suggesting that they should be avoided no matter what but that they should be reserved for sever bacterial infections and only after prior assessment by a medical practitioner.
If you are taking antibiotic minimise their detrimental impact on your gut flora by taking saccharomyces boulardii 6 hours after taking your medication for the duration of the course. Follow with a daily probiotic supplement containing Lactobacillus rhamnosus GG for 3 to 6 weeks. Those have been shown to greatly minimise symptoms of antibiotic induced diarrhoea. If you get thrush look for Lactobacillus reuteri RC-14 and Lactobacillus rhamnosus GR-1 as the most effective stains to protect against vaginal yeast infections.